INTRODUCTION
Odontoma is the most common type of benign odontogenic tumor, and often causes disturbances in the eruption of its associated tooth. Odontomas usually occur in the permanent dentition, and rarely occur solely in the primary dentition and account for 22% of the odontogenic tumors. Compound odontomas manifest as a regularly shaped, solitary or multiple small tooth-like denticles, where all dental tissues are represented in a structural and more orderly pattern. The term ‘odontoma’ was coined by Paul Broca in 1867. He defined the term as tumors formed by the overgrowth or transitory of complete dental tissue. Odontomas are probably a hamartomatous malformation of functional ameloblasts and odontoblasts rather than true neoplasms. The etiology is not clear, although local trauma, infection and genetic factors have been suggested as possible causes. A complex odontoma presents as an amorphous conglomeration of dental tissues consisting of enamel, dentin, cementum, pulp, and enamel organ. Peripheral compound odontomas
are rare, arise extraosseously, and have the tendency to exfoliate.
DEFINITION
The term odontome by definition refers to a tumor of odontogenic origin. In a broad sense, it means a growth with both the epithelial and mesenchymal components ex-hibiting complete differentiation with the result that func-tional
ameloblast and odontoblast form enamel anddentin. This enamel and dentin are usually laid down in an abnor-mal pattern because the organization of odontogenic cells failed to reach the normal state of morphodifferentiation. WHO
classification defines this lesion as ‘a malforma-tion, in which all the dental tissues are represented, individual tissues being mainly well formed but occurring in more or less disorderly pattern’.1
FEATURES
Odontomas are usually detected in school-age children, and the mean age at the time of diagnosis is 14 years .234 The majority of compound odontoma cases (74.3%) are diagnosed before the age of 20 years, during routine radiographic
examination, occurring commonly in the anterior maxillary region, without any gender bias. Odontomes are considered as the developmental anomalies resulting from the growth of completely differentiated epithe-lial and mesenchymal cells that give rise to ameloblast and odontoblast. These tumors are formed of enamel and dentin, but they can also have variable amount of cementum and pulp tissue. Odontomes by definition alone refers to any tumor of odontogenic origin.
Classification
According to W.H.O. classification,1 odontomes can be di-vided into three groups:
1. Complex odontome - when the calcified dental tissues are simply arranged in an irregular mass bearing no mor-phologic similarity to rudimentary teeth.
2. Compound odontome - composed of all odontogenic tissues in an orderly pattern that results in many teeth-like structures, but without morphologic resemblance to normal teeth.
3. Ameloblastic fibro-odontome - consists of varying amounts of calcified dental tissue and dental papilla like tissue, the later component resembling an ameloblastic fibroma. The ameloblastic fibro-odontome is considered as an immature precursor of complex odontome. According to Thoma and Goldman: 5
• Geminated composite odontomes - two or more, more-or-less well-developed teeth fused together.
• Compound composite odontomes - made up of more-or-less rudimentary teeth.
• Complex composite odontomes - calcified structure, which bears no great resemblance to the normal ana-tomical arrangement of dental tissues.
• Dilated odontomes - the crown or root part of tooth show marked enlargement.
• Cystic odontomes - an odontome that is normally en-capsulated by fibrous connective tissue in a cyst or in the wall of the cyst.
TYPES
There are essentially two types of odontomes:
1. Complex composite odontome;
2. Compound composite odontome. A new type known as Hybrid odontome is also reported by some authors “Complex
Composite Odontome”
COMPOUND COMPOSITE ODONTOME
The WHO classification defines this lesion as ‘a malforma-tion in which all the dental tissues are represented in a more orderly pattern than in the complex odontome, so that the lesion consists of many tooth-like structures. Most of these
structures do not morphologically resemble the teeth in the normal dentition, but in each one enamel, dentin, cementum, and pulp are arranged as in normal tooth’. The literature is flooded with a number of interesting case reports. Herrman
(1957) reported a case of compound composite odontome, which contained 2000 denticles. Multiple compound odontomes of maxilla and mandible were reported by Thomson et al. in 1968. Manil (1974) used the term odontome syndrome in a case that had multiform odontome both in maxilla and mandible. The majority of odontomas are associated with impacted teeth. Chang et al.6 found that the maxillary central incisor was most commonly involved. In this case, but the development of the maxillary right and left central incisors were affected. Regezi et al. in their review
of 706 cases of odontogenic tumors found that odontomes comprised of approximately 65% of odontogenic tumors making them the commonest type.7 Philipsen, Reichart and Praetorius reported the incidence of compound odontome between 9 and 37%, and the incidence of complex odontome between 5 and 30%.8
ETIOLOGY
The exact etiology of odontome is unknown9,10. The etiology of odontomas has been attributed to various pathological conditions like: Local trauma, inflammatory infectious process,9 hereditary anomalies (Gardners syndrome,
Hermanns syndrome), odontoblastic hyperactivity and alterations in the genetic component responsible for controlling dental development, a number of factors including prior trauma and infection seem to be involved.11A case of
compound odontoma associated with a history of trauma in the anterior region of the face in a 10- year-old was reported by Iturri et al.12 The persistence of a portion if lamina may be an important factor in the etiology of a compound or
complex. Hitchin suggested that the odontomas are inherited through a mutant gene or interference. When these buds are divided into several particles they may develop individually to become numerous, closely positioned malformed teeth or tooth-like structure. When the buds develop without such uncommon division and consists of haphazard conglomer-ates of dental tissues, they may develop into complex odontome. However the transition from one type to another is commonly associated with varying degrees of morphodifferentiation or histodifferentiation or both, and it is often difficult to differentiate between both the types.13,14 Recently, Philipsen et al.,15 put forth the hypothesis that for-mation of a compound odontome is pathogenically related to the process producing hyperdontia, ‘Multiple Schizodontia’ or locally conditioned activity of dental lamina.
OCCURRENCE
The compound odontoma is slightly more common than the complex odontoma, which in turn is more common than the ameloblastic odontoma. It is of interest to note that the majority of odontomas in the anterior segment of the jaws are compound composite in type (61%), whereas the majority in the posterior segment is complex composite in type (34%). interestingly, both type of odontomas occurred more frequently on the right side of the jaw than on the left. (Compound
62%, Complex 68%) E There is no gender predilection and odontomas can occur at any age.
CLINICAL FEATURES
Clinically, odontomes are generally asymptomatic; usually remain small, rarely exceeding the diameter of the tooth. Occasionally they do become large and may produce expan-sion of bone with consequent facial asymmetry. This is par-ticularly true if dentigerous cyst develops around the odontome. Signs and symptoms associated consist of unerupted teeth or impacted teeth, retained deciduous teeth, swelling and incidence of infection.9 The most common location for impacted teeth associated with odontomes is the anterior maxilla. Commonly compound odontoma (intraosseous) is located between the apex of a primary tooth and the crown of a permanent tooth preventing the eruption of the latter.
HISTOLOGICAL FEATURES
The tissue are processed and stained with hematoxylin and eosin stain. The stained section reveals, mature tubular dentin, enclosing hollow circular structures. These hol-low structures contain enamel that is lost during de-calcification.
Histologically, it represents the normally organized tooth structure, like enamel, dentin, pulp, and cementum including the periodontal ligament. A thin layer of cementum is present at the periphery of the mass.
RADIOGRAPHIC FEATURES
A presumptive diagnosis of compound odontoma is usually determined by radiographic appearance alone and is seldom confused with any other lesion.16 Radiographically odontomas present as well-defined, radio-opacities situated
in the bone, but with a density that is greater than bone and equal to or greater than that of a tooth. Radiolucent halo, typically surrounded by a thin sclerotic line, surrounds the radio-opacity. They are discovered on radiographs either incidentally or in search of a cause for a missing tooth.12 The radiolucent zone is the connective tissue capsule
similar to that of the normal tooth follicle is also surrounded by narrow radi-olucent rim and shape surrounded by a narrow radiolucent zone.
TREATMENT
Odontomes are treated by conservative surgical enucleation and there is little possibility of recurrence 17 Kaban states that odontomas are easily enucleated, and adjacent teeth that may have been displaced by the lesion are seldom
harmed by surgical excision because they are usually sepa-rated by a septum of bone.13,18 An odontoma has a limited growth potential, but it should be removed because it con-tains various tooth formulations that can predispose to cys-tic
change, interference with eruption of permanent teeth and cause considerable destruction of bone. Literature re-view suggests that radiographic examination of all pediatric patients that present clinical evidence of delayed perma-nent tooth eruption or temporary tooth displacement, with or without history of previous dental trauma should be per-formed. Early diagnosis of odontomas allows adoption of a less-complex and less-expensive treatment and ensures bet-ter prognosis.
CASE REPORT
An 11-year-old Sikh girl reported at Department of Orthodontics, Himachal Institute of Dental Sciences Poanta Sahib with chief complaint of irregular teeth. On extra oral examination, no obvious disfigurement of face was noticed (Fig 1). Parents were unaware of missing upper left lateral incisor. Intraoral examination revealed that upper left lateral incisor
was missing while right lateral incisor was erupted and well accommodated (Fig 2). A well defined swelling was present on labial aspect of 22 and 23, measuring about 1 x 1.5 cm, extending mesiodistally from distal of left central incisor to distal of over retained deciduous lateral incisor. Superioinferiorly it extended approximately 1 mm above
the marginal gingiva in relation to 21 to the vestibular depth. Overlying mucosa was slightly blanched (Fig 1,2). A white spot was visible distal to the swelling and no intraoral sinus or secondary change was seen over the swelling. There was gingival hypertrophy on distal aspect of 21. No inflammation of marginal gingiva and interdental papilla was present. The patient was fit and well medically. Extra oral examination was unremarkable. On palpation, swelling was bony hard in consistency, non-tender, well defined, fixed to the underlying tissue, and was not mobile. Palpation over white spot suggested erupt-ing tooth (Fig 2).Palatal aspect in relation to 23 and 22 was normal. The appearance of her teeth was a concern but she had no complaint of pain or previous infection. Patient’s family history was non-contributory.
 | Fig 1. Extra-oral pictures of the patient
 |
 | Fig 2. Intra-oral pictures before surgery. Note blanching of mucosa due to underlying odontoma
 |
calcified mass was present over the root apex and distal aspect of 22, resembling enamel and dentin. Root in this tooth-like structure was not clearly visible. A thin radiolucent line covering this toothlike structure was also present.
The patient was prepared under local anesthesia (2% lignocaine 1:80,000 adrenaline). A crevicular incision was made in relation to labial aspect of 21, 62 and 63, followed by two diagonal relieving incisions (Fig 5). To facilitate proper
access to site, 62 and 63 were extracted. The mucoperiosteal flap was elevated towards the lateral aspect of maxilla, which initially revealed the presence of one of the most prominent denticles (Fig 4,5). First of all the most prominent
denticle was removed carefully so as not to injure the adjoining unerupted permanent teeth. The remaining bulk was a fused mass of denticles out of which one got detached and extracted separately. This remaining mass became mobile
on slight elevation, but could not be delivered; therefore it had to be cut into two pieces with the help of carbide surgical bur. This facilitated removal of the calcified mass without injuring adjoining unerupted permanent teeth. The
extraction socket appeared normal (Fig 5). The area was curetted gently and sharp bony margins were rounded off, the area was irrigated with Normal Saline solution, and the flap was placed back and held in position with the help of 3-0 silk
sutures. Macroscopically, the specimen consisted of many pieces of irregular denticles (Fig 6). The
 | Fig 3. A. Digital OPG showing odontoma blocking eruption of 22 and 23 B. Close-up enlarged view
 |
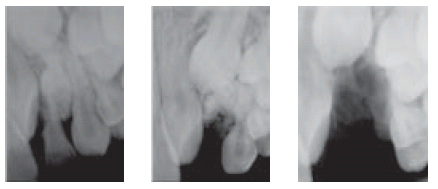 | Fig 4. A. Intra-oral digital X-ray before surgery B. After removal of one big denticle C. Post extraction socket
 |
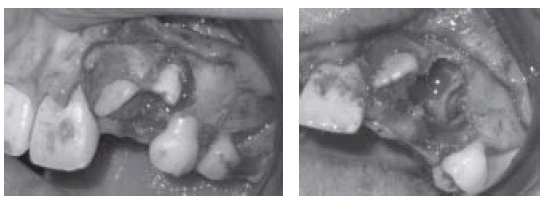 | Fig 5. A. Surgical exposure of the odontome B. Socket after extraction of the odontome
 |
 | Fig 6. Close-up view of extracted denticles
 |
 | Fig 7. Histo-pathological section showing demineralised denticles
 |
recovery was unremarkable. Patient was recalled for removal of sutures after one week and follow up check up after 6 weeks. The surgical area appeared absolutely normal (Fig 8). Histological sections showed both tooth like
and haphazard arrangement of dental hard and soft tissue including cementum, dentine, enamel matrix, pulp and periodontal tissue. The pathology report was consistent with a compound odontome (Fig 7).
REFERENCES:
1. Kramer IRH, Pindborg JJ, Shear M. Histological Typing of Odontogenic Tumour. WHO. International Histological
Classification of Tumours; Second Edition; Berlin Springer 1992:16-21.
2. Kaugers GE, Miller ME, Abbey LM. Odontomas. Oral Surg 1989;67:172–6. [PubMed]
3. Tandon S, Radhika M. Compound composite odontoma in primary dentition – A case report. J Indian Soc Pedod Prev
Dent. 1998;16(4):111–4. [PubMed]
4. Kaneko M, Fukuda M, Sano T, Ohnishi T, Hosokawa Y. Microradiographic and microscopic investigation of a rare
case of complex odontoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:131–4. [PubMed]
5. Thoma KM, Goldman HM. Oral Pathology, 5th edn. St Louis, The CV Mosby Company 1960. p. 1221-2.
6. Chang J Y, Wang J T, Wang Y P et al. Odontoma: a clinicopathologic study of 81 cases. J Formos Med Assoc
2003; 102: 876–882. | PubMed |
7. Supriya Pande, Ganvir SM, Hazarey VK. Recurrent Odontome-A Rarity. JIDA 2003;74:115-8.
8. Philipsen HP, Reichart PA, Praetorious F. Mixed Odontogenic Tumors & Odontomas. Considerations on Interrelationship. Review of Literature and Presentation of 134 New Cases of Odontomas. Oral Oncol 1997;33:86-99.
9. Shafer. Hine and Levy: A Text Book of Oral Pathology; Fourth Edition; W.B. Saunders & Co 1993;308-12.
10. Kramer IRH, Pindborg JJ, Shear M. Histological Typing of Odontogenic Tumour. WHO. International Histological
Classification of Tumours; Second Edition; Berlin Springer 1992:16-21.
11. Ferrer Ramirez M, Silvestre Donat F, Torres-Gomez F J, Avella-Vecino F, Salazar-Fernandez C. Recurrent infection
of a complex odontoma following eruption in the mouth. Med Oral 2001; 6: 269–275. | PubMed | ChemPort |
12. Samano Iturria G, Cedeno Pacheco E. Compound odontoma with history of trauma: a report of a case. Pract Odontol 1988; 9: 18–20. | PubMed | ChemPort |
13. Batra Puneet, Gupta Shweta, Rajan Kumar, Duggal Ritu, Hariparkash. Odontomes-Diagnosis and Treatment: A Case Report; JPFA 2003;19:73-6.
14. Piattelli A, Perfetti G, Carrano A. Complex odontome as a periapical and interradicular radioopacity in a primary molar. Journal of Endodontics 1996;22:561-3.
15. Philipsen, HP, Reichart PA, & Praitorius F: Mixed odontogenic tumours and odontomas. Considerations on
interrelationship. Review of the literature and presentation of 134 new cases of odontomas. Oral Oncology 1997; 33(2):86-99.
16. Neville BW, Damm DD, Allen CM, & Bouquot JE: Oral and Maxillofacial Pathology. 2nd ed. (9.) Iannucci-Haring J: Case study #7. RDH 1990; 10:10,12. Philadelphia, WB Saunders Co., 2002, p. 626-32.
17. Areal-Lopez I, Silvestre DF, Gil LJU. Compound odontome erupting in the mouth; four year follow up of a clinical case. J Oral Pathol 1992;21:285-8.
18. Kaban LB. Pediatric Oral and Maxillofacial surgery Philadelphia:Saunders; 1990. p. 111-2. |